Blue Tarps, Generators, and the Coqui: Puerto Rico Gives New Meaning to Resiliency

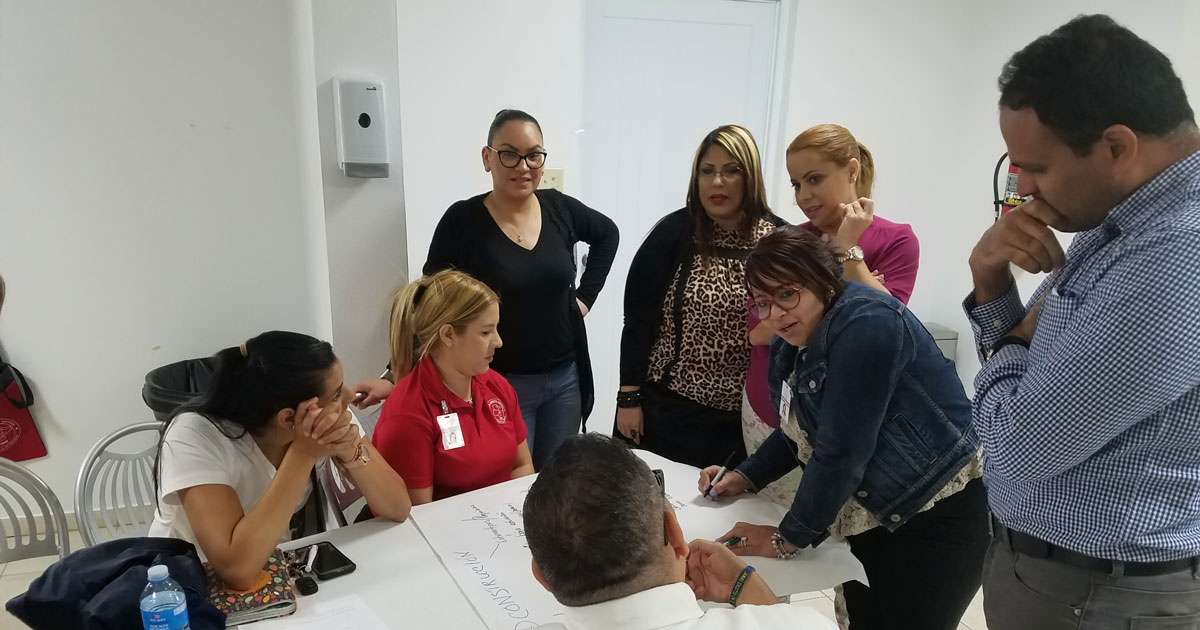
Photo: Corporación de Servicios Médicos (CSM)
By Amy K. Liebman, MPA, MA
Tired. Sad. Strong. These were just a few words that came to mind as I looked at my friend and colleague, Dr. Jose Rodriguez, as he welcomed me to Puerto Rico. I’ve been working for over a decade with Dr. Rodriguez, the medical director for the community health center, Hospital General Castañer, nestled in the mountains of central Puerto Rico. Now, our work continues. It’s my first time back since Hurricane Maria, a Category Five hurricane that devastated the island six months ago, leaving millions without power, disabling communication, destroying water systems and ripping the roofs off of thousands of homes. Dr. Rodriguez invited Migrant Clinicians Network to work with health centers and other groups across the island to facilitate a continuing education event, entitled, “Learning From the Past and Looking Ahead to the Future -- Natural Disasters and Our Patients.” We also continued our partnership with his health center to train workers about health and safety as they clean up and rebuild the island. In all, we traveled over 300 miles and worked with nearly 100 clinicians from 17 health centers in various remote locations across the island. Alma Galván, MHC, a fellow MCNer, along with Dr. Rodriguez and Dr. Lorena Torres, a clinical psychologist, and the Puerto Rico Primary Care Association, facilitated the workshops where we looked at vulnerability, occupational and environmental health, chronic disease management, and traumatic stress.
Like many trainings I’ve helped to facilitate over my career, I walked away learning so much more than I could ever offer. The workshops on the disaster brought together frontline providers from across the island. For many, it was the first time in a safe, structured training environment where they were asked to share with their colleagues their experiences of searching for patients, caring for those in need, and figuring out best practices after the hurricane. Many of the most vulnerable communities were completely cut off and providers shared their determination and creativity to “bring the health center to the community.” Corporación de Servicios Médicos (CSM), a community health center in Hatillo, hosted our first workshop. Executive Director Armando Legarreta Raices opened the workshop, reminding all of us of the role of the health centers to “serve as a bridge to the community.” As Dr. Figueroa, CSM’s medical director, pointed out, “We knew our community before the storm,” making it possible to find them and care for them after the storm.
As the weeks drag into months, the slow and harsh recovery process is taking its toll. There is a sadness, an unhappiness, “como triste” as borinquens call it. Post-Maria mental health needs were both expected and overwhelming. As confirmed over and over again by the clinicians with whom we worked, mental health continues to be a central public health concern. See NPR’s recent discussion with clinicians from Castañer.
As Alma and I traveled across the island to our workshops in Castañer and Ponce, the catastrophic convergence, compounding and amplifying deep-seated problems, became alarmingly clear. The island’s infrastructure, poorly maintained largely as a result of an economic policy of fiscal austerity, simply cannot rebound quickly from the blow of Maria. And so many families, already in poverty, endure further hardship. Homes remain without running water and electricity. The sound of generators, for those fortunate to have them, permeate the countryside, competing with the croak of the island’s renowned coqui frog. Blue tarps dot the landscape, marking the homes with damaged roofs. Potholes litter the roads. The fincas of oranges, platanos, and coffee are mangled and bare. The fragility of the island’s infrastructure became ever so apparent as we experienced a total island black out. The cause: a backhoe damaged one line. Yes, one line and the island became dark. Our daylong workshop on the day of the blackout delayed our arrival to Ponce, a small city on south part of the island. As Alma and I drove through the city center it was completely dark. Few lights flickered in the homes and not one street light showed us the way. With little trust in the power company that electricity would return within the promised 36 hours, communities prepared for the long haul as grocery store shelves emptied and lines for gasoline to power generators formed. Community members trickled into the generator-supported clinics, plugging in respirators and cell phones. To make matters worse, the island-wide power outage came at the same time as torrential rains pelted parts of the island. As an nurse from one community health center stated, “The blackout brought it all back. It felt like a mass PTSD.”

But the scale of the damage has taken a marked toll on the clinicians as well, who are tasked not only to care for themselves and their families, but the whole community. Our partner health centers in Puerto Rico already care for the island’s most vulnerable. In the aftermath of the storm it was the community health centers, these stand-alone institutions governed by the community and supported in part by the federal government, that emerged as the true leaders of the response. They made sure their patients were accounted for. They knew who needed help with their breathing machines, who needed medicine, and who lived alone. They trekked to the most remotely located homes, in some cases wading through streams to get to their patients. When help from the outside was slow to trickle in, the health centers were already there. They served as “central command,” even offering abbreviated banking services, as other basic services were painfully slow to come back online.
Alma and I were reminded not only of the strength and resilience displayed by those on the frontlines, but of the traumatic stress our partner clinicians endured and are continuing to endure. As they care for the most vulnerable, they, too, suffer. Many providers from outreach workers to physicians lived for months without lights. Several clinicians told us they lost their homes, they lost everything. One physician whose home was completely destroyed noted, however, that “while the rest of the world looks at us as poor Puerto Ricans, I see strength. We are not poor. We are Puerto Rico strong!”

Dr. Rodriguez wrote about his experience in the midst of the alarmingly weak response from government agencies: “I am proud of how my colleagues and the local citizens have pulled together and largely pulled ourselves up by our bootstraps. And I am dismayed at the paltry response from municipal, state, or FEMA authorities. Nine weeks after the hurricane, our town is still without electricity, water, internet, or phone service. The hospital continues operating every day around the clock, and we are slowly recovering almost entirely on our own. If help comes, we will welcome it, but we know we cannot wait for it.The community is proud of its hospital — and for that we keep working.”
As facilitators from the “mainland,” Alma and I clearly acknowledged and recognized that Maria was their experience. Our co-presenters, who lived through Maria, offered important content to consider regarding chronic disease management and traumatic stress based on the best practices and lessons learned from the storm. What we offered and participants welcomed was the framework that Alma put forth to work through together what had happened, find the lessons in there, and begin planning for the future. And planning is needed even as the island is still deep in the recovery and rebuilding phase. As Dr. Rodriguez and several clinicians noted, all centers have plans, they just didn’t work in a case when all communication systems are wiped out. As planning efforts re-emerge with hurricane season around the corner, the question remains: How do frontline clinicians prepare? What is abundantly clear is that more support and assistance are needed. We need to build from the lessons learned and from the demonstrated resilience of this incredibly vulnerable yet strong island.
Community health centers are true leaders. We at MCN are proud and honored to continue this important process and our joint efforts to support our Puerto Rican partners as we move ahead to prepare for the next season of storms.
Like what you see? Amplify our collective voice with a contribution.
Got some good news to share? Contact us on our social media pages above.
Return to the main blog page or sign up for blog updates here.
- Log in to post comments