Transnational Tuberculosis: Q&A with Dr. Cynthia Tschampl
 Last week, a newly published paper indicated that over 2,800 people leave the United States with active tuberculosis (TB) each year, while only ten percent receive continuity of care services like those provided by Migrant Clinicians Network’s Health Network. Without bridge case management, such cases could lead to incomplete treatment and development of drug resistance. The article, published in Emerging Infectious Diseases, concluded that the most effective policy response may be to make case management systems like Health Network and San Diego Public Health Services’ CureTB available to all referring clinicians with patients suffering from TB.
Last week, a newly published paper indicated that over 2,800 people leave the United States with active tuberculosis (TB) each year, while only ten percent receive continuity of care services like those provided by Migrant Clinicians Network’s Health Network. Without bridge case management, such cases could lead to incomplete treatment and development of drug resistance. The article, published in Emerging Infectious Diseases, concluded that the most effective policy response may be to make case management systems like Health Network and San Diego Public Health Services’ CureTB available to all referring clinicians with patients suffering from TB.
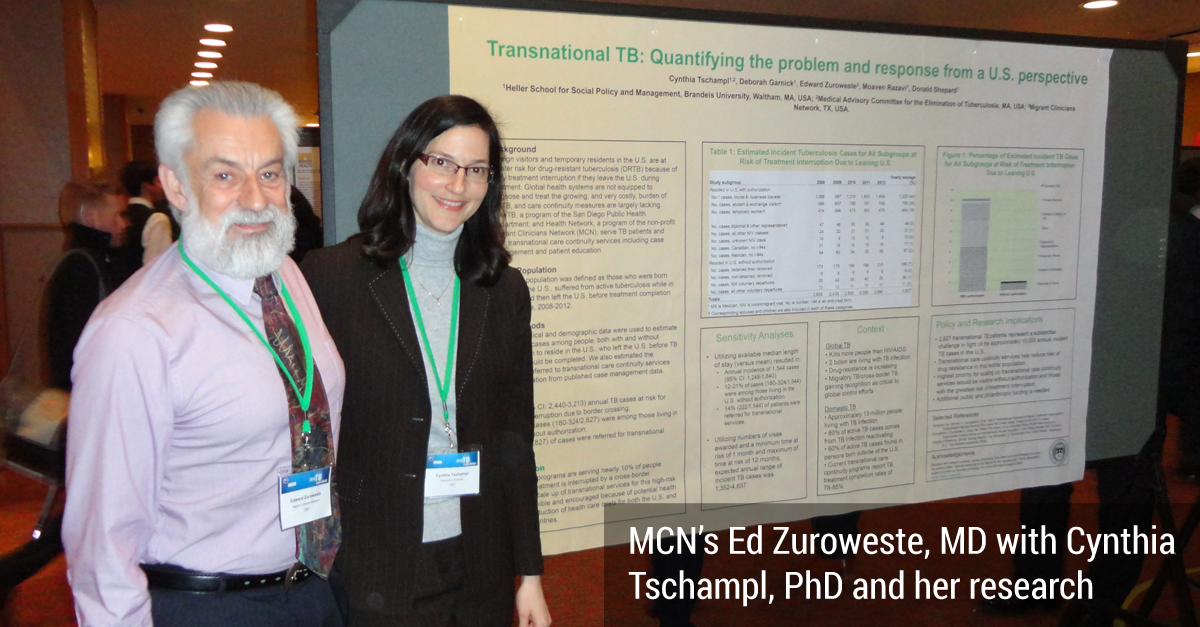
What does this research mean in the larger context of our fight against TB? And what does it say about Health Network? To learn more, I reached out to Cynthia Tschampl, PhD, the lead author of the paper, who has worked closely with Migrant Clinicians Network to evaluate Health Network and its effectiveness, and who is deeply involved in work to eliminate TB, to learn more about her path in studying TB, her current research, and her perspectives on the mycobacterium that infects one in three people on the planet.
CS: How did you first become interested in tuberculosis?
CT: I was a volunteer with RESULTS, my favorite anti-poverty organization. I’ve been volunteering with them since 2000. The way they choose the campaigns that they work on is a three-part analysis. The first one is, what are the things causing the most hunger and poverty in the world and in the United States? The second analysis is, what are the things that are actively making an impact against hunger and poverty? And thirdly, where can we as a coordinated group of individuals -- a small but coordinated group -- make an actual impact?
With that triple-analysis, they picked up TB as an issue in 1996. That’s because it was utterly clear, even back then that TB caused poverty, as well as was fostered by poverty. Furthermore, internationally, sixteen bucks worth of drugs would save these people’s lives because TB is preventable, treatable, and curable.
TB also mostly kills breadwinners in the prime of their lives, so they lost all that productivity, and thinking of an average family of five, you don’t just lose the income of one person who is most likely to die, you plunge a family of five further into poverty.
Consistently, the global burden of disease reports say that TB is the most cost-effective intervention on the globe. It’s been consistently found to be both a retardant of economic progress, and when we prevent or cure TB, then that proves to be a boon to your underlying economic levels.
Because of my advocacy work on TB with RESULTS, I was recruited to sit on the Massachusetts Medical Advisory Committee for the Elimination of Tuberculosis (MACET). That was in 2004.
I was working on domestic TB quite a bit, and then I started graduate school, and they asked me to pick a concentration, and I thought, well, I have this eight-year background on tuberculosis, let me apply to the health concentration. I then did most of my coursework writing on some aspect of TB.
CS: This week, you published one of three papers that you worked on for your PhD. How did you decide to write about Health Network, to focus on case management of TB in your dissertation?
CT: If you ask a hundred PhDs, you’ll get a hundred different answers. The best word I can give you is, “iterative.” You explore research topics, and you explore data sources, and you talk to people because you have to find a chair and people to serve on your committee.You have to find a fit with all of those moving pieces. Meanwhile, I never stopped volunteering for RESULTS, I never stopped volunteering for the MACET, I continued to go to the annual meeting of The Union (International Union Against TB and Lung Disease)-- North America Region (NAR), presenting on the MACET work or my research. I kept my ear to the ground. I had a couple of conversations with Del and Ed [from Migrant Clinicians Network] and they were excited about using their data, because they are [focused on] the patient care side of things, the service delivery side of things, and it seemed they didn’t really have the staff to do the research, so it seemed like a good symbiotic match.
I mapped out the three-paper dissertation, with three separate questions and three separate methodologies, [using] some of the same data [for all three]. I contacted the Department of Homeland Security to use data on active TB cases that they referred to Health Network for transnational case management, but we were not able to confirm permissions in the time I had allotted to complete my dissertation.
The first paper -- the one that just got published -- is really an epidemiological estimate, and it was mostly independent of Health Network’s data [so it was not affected by the lack of Department data]. For the other two papers, one was looking at the characteristics of treatment completion and survival rates for MCN’s served TB infection population, and the third one used the same population [to explore] the cost-effectiveness of the Health Network bridge case management program.
So we did a pivot [for the second and third papers], and we asked the same questions, and [used] the same methodology, [but moved] from the transnational active TB cases to the domestically-mobile TB infection cases [as those were not cases from the Department of Homeland Security]. And all of it worked out. I did the proposal defense, and I got green lights across the board, so we proceeded.
CS: Were you surprised by any of the results?
CT: Yes. I was surprised. First of all, the magnitude of the number is surprising, in the epidemiological study. When you [see] that we’re estimating 2,800-plus cases a year that are activating and leaving the country, and you compare that to the overall burden of about 10,000 cases that are reported on the official CDC report every year, it makes you wonder, how many cases are we really missing? This is an epidemiological estimate and a way to begin the conversation about the missed opportunity, because the majority of these folks are much more vulnerable to drug treatment interruption, which will lead to more drug resistance.
Since we have clearly documented that the global health systems cannot handle the current burden of drug-resistant TB, it behooves both the US and the receiving countries to get on top of this. When you have more of these people enrolling in transnational care continuity services like Health Network and CureTB, you have better surveillance data, you have them on record as having completed or not -- for the most part, some are lost to follow-up -- but the numbers are quite good, given the mobility issue…
[Many of these patients leaving the country with active TB] come back to the United States. One MMWR citation in the first paper said that about 25 percent of people without authorization to enter the US would come back.
And for the population with visas who come in an authorized manner, a lot of them are students -- they’re going to come back for a number of years consecutively to finish their degrees. [People with] business visas, they’re [permitted] multiple entries, so they just come and go.
So. there is a portion [of this] that is purely in the self-interest of the United States. But if we can contribute, because we have the resources, to the global surveillance and global control of TB, particularly in this space, this really tough-nut-to-crack space of transnational or cross-border or mobile TB, however you want to call it, it’s going to help everybody.
CS: What do you hope happens as a result of your research getting out there?
CT: So many things! It’s really an extension of everything I’ve been working toward. The big goal, the eye on the prize has always been and forever will be TB elimination. Just [as was] reiterated time and time again at the NAR meeting in Denver, prevention is going to be a huge piece of this. So to the extent that my research helps demonstrate that programs like Health Network can help increase TB prevention prophylactic courses, that’s great, because we really have to demonstrate and scale up in a big way treatment of TB infection if we’re ever going to move in the direction of TB elimination, much less get there.
There are positive things that will happen as corollaries en route to TB elimination. This is one of those cases where a fairly downstream intervention really does help with health inequalities and income disparities and health disparities. Because TB is such a strong cause of poverty -- it’s not just that poverty fosters TB -- it has that much potential for economic impact. It’s the leading infectious killer in the world. One in four people with HIV/AIDS will die of tuberculosis. And it’s preventable, it is treatable, it is curable. Those characteristics should never go together. We should’ve beat this thing awhile ago! It’s tremendously widespread.
CS: Do you want to speculate why it’s taking so long to get rid of TB?
CT: Part of it is that the bug is evolving. It’s been around since human civilization. It’s developed specific biological characteristics that really make it tough to kill. The other thing is we did make a lot of mistakes with our early antibiotics/early treatment with antibiotics, because we developed drug resistance. Early drug-resistant TB was almost entirely man-made, from what I understand. I’m not a basic scientist, but from everything that I’ve read... that’s my understanding. Now [drug resistance] is propagating on its own.
And if you look at the level of investment in TB you see a dramatic under-funding in research and development. We’re still using a diagnostic tool that’s 130 years old. The TB skin test is 130 years old. What other condition in modern medicine do you have that uses a diagnostic that’s over 100 years old? That’s an indication of how neglected this space has been.
It’s also so widespread because it’s airborne, that’s another evolutionary thing about the bug that makes it tough. We as a society didn’t catch up…. We have approximately two billion people infected. We have this huge reservoir of infections that we need to start dealing with if we’re going to get to TB elimination.
CS: It sounds complicated.
CT: Every conference I go to, every scientific presentation, pretty much everything I read about tuberculosis, [they] consistently reinforce just how complex this bug is. The transmission, the number of resistant strains -- the sheer number of TB strains out there -- it’s overwhelming in some ways. The diagnostics are imperfect, the treatments -- when we’re talking about getting to the level of MDR- and XDR-TB, the treatment is inhumane, because the medicines are so toxic. It has been a disease and a public health issue marked by neglect at every single stage.
[In Massachusetts,] we have an unbelievable burden of drug resistance. One in four is resistant to one drug, and we had a record-breaking year on MDR-TB. We’re now four times the US average for MDR-TB. Our rate is actually higher than the global average!
CS: How does this research link in with the White House’s recently released National Action Plan Combating Multi-Drug Resistant Tuberculosis (NAP)?
CT: The first paper really focuses on a key group of ‘how we can avoid drug resistance from being developed in the first place,’ because the NAP is really focused on drug resistance... There’s very much this effort toward, okay, we can’t handle the current global load of drug resistance we have, and we need to be really intensive and purposeful in preventing more. But we don’t even have the basic epidemiological understanding of what the magnitude of the problem is, so that first paper was key in shedding light on the situation and getting more situational awareness.
The other two papers, while they focused on TB infection, [they are] particularly helpful in the space of describing and beginning to quantify the Health Network bridge case management system. We know that it’s being used on active TB cases, which again, [features] people with a lot of vulnerabilities and active TB, and so far the reported completion rates are high. So those other two papers lay the groundwork in exploring whether this might be another useful tool in combating further development of drug resistance. Also, MCN’s Health Network is helping case manage a cross-country mobility of patients with drug-resistant TB, so if we can measure that as well… I don’t know if there are enough cases to do an individual analysis yet, but we have templates and the groundwork laid [to do that research in the future].
CS: What do you think TB will look like in ten years, and why? How optimistic are you?
CT: Oh, man. That question breaks my heart, because I am such an optimist, and I married an optimist, but I’m also a pragmatist. I have a pretty long record of looking at things as they are and always asking the ‘why,’ and trying to drill down for more and more facts, and getting an understanding of the facts, especially the context. And the task before us is enormous.
Given that the budgets -- both at the state level here in Massachusetts, [where] I’m most familiar... and at the national level, looking at President Obama’s fiscal 2017 proposed budget, I’m afraid that there isn’t as much cause for optimism as I would hope.
Some of the mathematical analyses presented at NAR suggested that if we are going to get to TB elimination, dealing with the active TB is almost secondary. We have to get into the reservoir of TB infection and we have to do it in a broader way than maybe anybody’s been talking about up to this point. When you look at the sheer mountain of work, it’s overwhelming.
On the other hand, there were pieces for optimism. One [was] that we have two new drugs for drug-resistant cases... There also is another class of drugs that may offer some assistance in the severely drug resistant [cases]... It is a cousin to penicillin, but it has a different action against the mycobacterium than penicillin does, and that’s why it’s effective and penicillin isn’t.
Another thing -- it’s such a small thing but it has the potential to make a big splash nationally -- is a new patient advocacy group, run by patients and/or people affected by tuberculosis, called We Are TB. The woman who is coordinating that is a powerhouse… and she will absolutely move and inspire you when she tells you the story of her two year old who was tremendously affected by TB and they couldn’t diagnose her for months.
I hang on to the hope that while the diagnosis is inadequate, and the treatment is inadequate -- in fact it’s punishing for the patient -- we do have what we need to get people to treatment completion and, for the most part, cure TB right now. And if we can have a multi-level push: more treatment of TB infection, more research on new drugs, more research on diagnostics, and, who knows, maybe even a vaccine that’s even partially effective because that would be a game changer… I think we can get there.
The other piece that was very encouraging was that the Stop TB Partnership presented… that the WHO is releasing a TB elimination plan that is more ambitious than it ever has been… It’s another sign of hope and another possible piece to the [puzzle]. Maybe we can put all these pieces together for significant progress moving forward. But I’m not going to lie -- it’s a big, big job.
CS: You mentioned We are TB. What other groups should we be watching?
RESULTS is still in there for the long haul, and they do great work. TB PROOF is moving forward to try to help prevent the health workers from getting TB. TB PhotoVoice empowers survivors to share their stories. There also may be something coming out of the countries most affected by Ebola because TB dramatically increased in those countries because of the diversion of resources toward Ebola… There’s a lot of good work out there.
I think it’s going to take a lot of combining these efforts and focusing especially on our decision makers and pursestring holders to give proper financial support that matches the magnitude of this problem, because we can’t really make meaningful progress until that happens.
Read Dr. Tschampl’s epidemiological estimate on people with active TB leaving the US in the current issue of Emerging Infectious Diseases. Hear about future publications of Dr. Tschampl’s work right here on MCN’s blog. Subscribe to our blog to get notifications of future installments.
- Log in to post comments