This pilot project was a collaborative effort involving project partners Futures Without Violence, Alianza Nacional de Campesinas, Líderes Campesinas, RAND, and Migrant Clinicians Network and was made possible with the support of California's ACEs Aware initiative through the UCLA-UCSF ACEs Aware Family Resilience Network (UCAAN) pilot program.
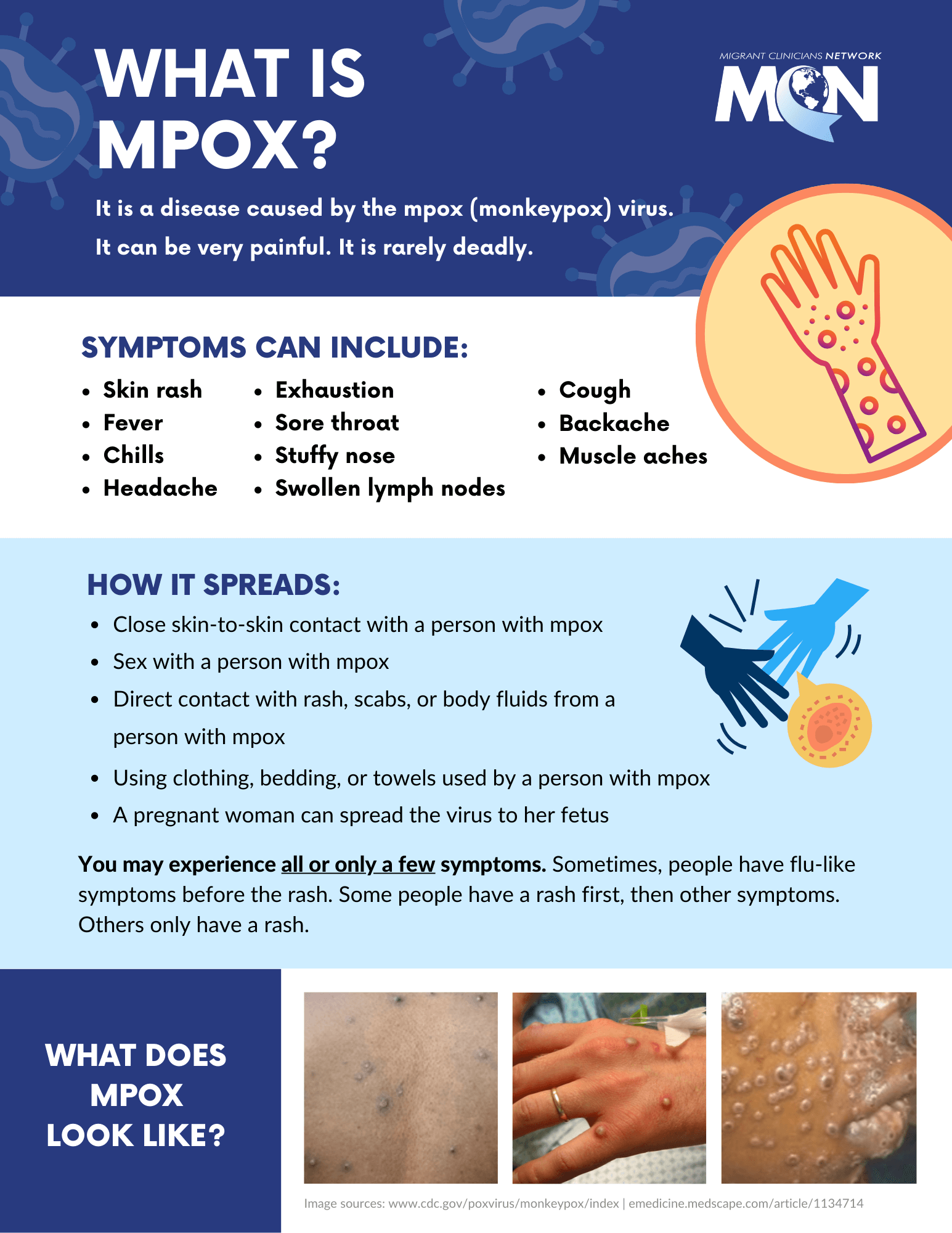
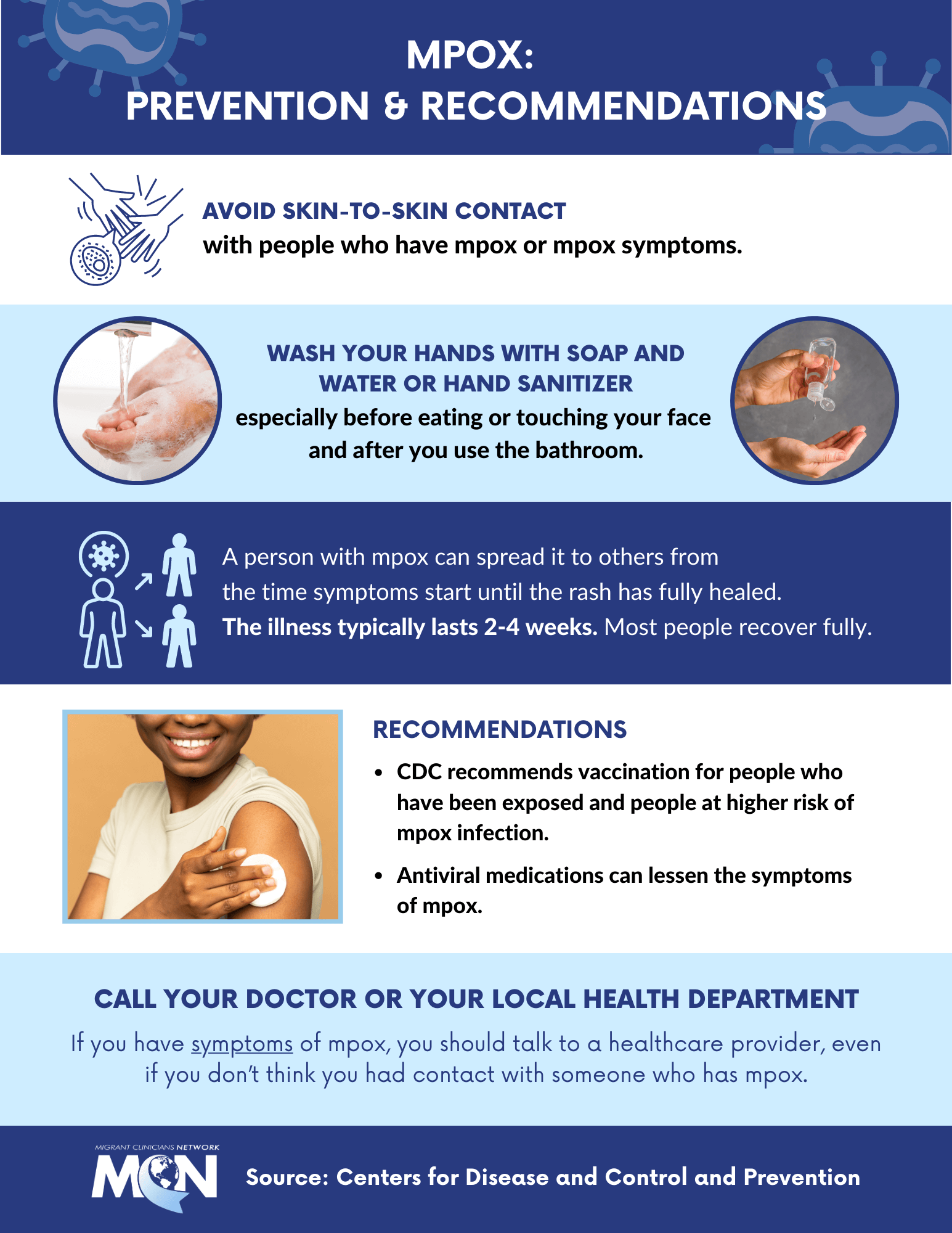
Education, screening, and response with evidence-based interventions are critical to addressing ACEs. However, ACEs education and screening that are culturally aware are not currently reaching farmworker communities in California. NACES aimed to increase opportunities for farmworkers to inform health care screening and responses to ACEs, increase ACEs education in farmworker communities, build partnerships between community health centers and community-based organizations, and ultimately improve access to care.
The project was divided into two parts, a community-based component presented in this report and a clinical component that examines how the results and recommendations of this community-based portion changed health center outreach, education, and response to ACEs. The community-based component was divided into two phases. Phase 1 involved the evaluation of farmworker leader training and Phase 2, the evaluation of the peer-led farmworker training.
The evaluation team employed a participatory action research (PAR) approach, developing instruments, presenting, and validating results with the partners to ensure active participation and collective action from all project partners and the farmworker leaders themselves.